News
Doctor's Advice

Our priority through this pandemic is the safety of our clients and patients. We are implementing new protocols to be able to provide you with the best veterinary care while maintaining the safety of everyone involved.
We are not closing currently. If the situation worsens or we are forced to close, then Dr. Jarvis will be available for emergencies.
Here are the policies we have implemented to help keep everyone healthy:
1) We ask if you are feeling ill, please have a neighbor or friend bring your pet in for their appointment.
2) We are offering curbside drop-off and pickup to maintain social distancing. To take advantage of this, please call the clinic, 928-284-2840, once you are in the parking lot for appointment. We will then send a technician out to get a history and bring your pet into the clinic. Once the examination is completed, we will call you with the findings and recommended diagnostics and/or treatment plan. When the appointment is finished, we will bring your pet back to you in the parking lot. A side note: While your pet is in the clinic, we can use Facetime or Skype so you can watch the examination, diagnostics, and treatments if you would like.
3) Taking the curbside drop-off and pickup one step further, we can do home pickup and drop-off as well. Again, we will not enter the home to help maintain social distancing. The home pickup an drop-off will flow like the curbside drop-off and pickup except we will come to you to pick up your pet and then bring your pet back home.
4) We disinfect every exam room after every appointment (this is standard daily protocol and not just COVID-19 protocol) and will continue to do so. We will also be disinfecting the doors, doorknobs, countertops, and lobby furniture multiple times throughout the day.
5) On the bright side, there is no evidence that pets can get COVID-19. There is no need to worry about your pet becoming infected.
6) As this pandemic ramps up and people start to become ill, we are offering boarding in an attempt to minimize pets being dropped off at the local shelters. If you become ill and can no longer care for your pet please contact us and we board them at the clinic until you are well again. We are here for the community and are willing to help wherever and however we can. We don’t want to see pets become homeless during this tough situation.
WE ARE NOW OFFERING TELEMEDICINE. This service is available to clients that have a current physical examination (i.e. we have seen your pet in the past year). This is state law and not our policy. To take advantage of the telemedicine follow the following steps:
1.) Load the Medici app on your smart phone or computer.
2.) Enter your location or allow your phone to use your location. You will then see a list of providers (both MDs and DVMs). Select Rachelle Jarvis.
3.) I will receive notification once you have selected me and then you will receive an invitation email. Once you are confirmed as a client you can then text and video your concerns and we will begin the telemedicine consultation.
4.) We won’t be able to provide everything through telemedicine but there is a lot we can do. If you have more questions regarding this service please give us a call 928-284-2840.
Please feel free to contact us with any questions or concerns that you may have. We are here to help.

Dilated cardiomyopathy (DCM) is a condition that causes the heart muscle to stretch resulting in a weak heart beat and poor profusion. DCM was very common in cats until 1987, when it was linked to a taurine deficiency. The DCM was reversed with taurine supplementation and now commercial diets all include taurine. DCM is now a rare disease in cats and mostly seen when they are being fed a vegetarian or home cooked diet.
Dilated cardiomyopathy can also occur in dogs. DCM has a genetic component in Doberman Pinschers, Saint Bernards, Irish Wolfhounds, and Great Danes. Recently, cardiologist have noticed higher rates of DCM in the breeds that do not have a genetic component. They have also noticed that the dogs that are developing DCM are on grain-free diets. These dogs also have their heart disease reversed with supplementation of taurine.
We do not yet understand why we are seeing an increase of DCM. What is known is that dogs with DCM are being fed a grain-free, vegan, or home-prepared diet. Diets that are grain-free usually have more potatoes, peas, lentils, or chickpeas to replace the grain. Could these ingredients be contributing to the issue? Or could it be that the protein source is usually exotic such as kangaroo, buffalo, or bison? It is known that kangaroo meat has low levels of taurine. Is it the ingredients within the diet or the lack of taurine causing the heart disease? What is known is that the heart disease is generally reversible with taurine supplementation.
What should you do with this information? If you are feeding a grain free diet you might want to reconsider. There is no scientific evidence that grains contribute to any health problems in our pets, although an internet search may say otherwise. I would recommend feeding a diet from a company with a long track record of producing good quality diets that has excellent nutritional expertise and rigorous quality control standards.
If your dog is diagnosed with DCM and they are eating a grain-free, vegan, or home-prepared diet I would recommend changing their diet to a well-known reputable company. Have the plasma taurine levels checked (this is a simple blood test) and begin supplementing with taurine. It will take 3 to 6 months to see any improvement with the DCM. Also make sure you are giving the prescribed heart medications to treat the disease.
The FDA has released a statement regarding this current issue and it can be found on Bell Rock Veterinary Clinic’s facebook page. You can also visit acvn.org to find a veterinary nutritionist. Please speak with your veterinarian if you have any questions or concerns regarding your pet’s dietary needs.
I start my exam with the goal to localize the lesion. Her head, front legs, back legs, and tail all appear to be affected. I walk her up and down the hallway and watch her gait which is very stiff, and her tail is elevated. Her mentation is good, she is aware of what is going on around her and actually quite happy, she just doesn’t have control of her muscles and they are all in a state of contraction. My physical exam allows me to localize her lesion to the nerve junctions where neurotransmitters are released. I am sure I know what is going on; Jackie has tetanus.
Clostridium tetani is a bacterium that produces spores that persist for long periods of time in the environment. They enter a wound (her spay incision) and clinical signs appear 5 to 20 days after. Clinical signs range from a stiff gait, erect ears, an elevated tail, contraction of facial muscles, seizures, and death due to not being able to ventilate. The toxin spreads through the peripheral nerves to the spinal cord, where it blocks the release of neurotransmitters from the inhibitor interneurons thus causing the extensor muscles to stay in a state of contraction. Cats are more resistant to the infection than dogs are.
Jackie was placed on two antibiotics to treat the bacterial infection and made a full recovery, thankfully. She is a lively, happy, playful pup to this day.
If there are any topics you would like covered in this monthly article, please fill free to contact me and I will do my best to address them. I can be reached via email: drjarvis@bellrockvet.com or on our facebook page Bell Rock Veterinary Clinic.

I always recommend approaching anesthetic procedures with a risk versus benefit ideology. If the procedure’s benefits don’t outweigh the risk of the anesthesia then the procedure should not be done. Prior to anesthesia, the pet should receive a thorough physical exam and blood work. The blood work should include a complete blood cell count and chemistry panel to ensure that they can metabolize off the anesthesia and there aren’t any underlying issues.
All pets having anesthesia should have an intravenous catheter placed. The purpose of the intravenous catheter is twofold: first, intravenous fluids can be administered during the procedure to help maintain hydration and blood pressure. Second, if there is a reaction or complication the intravenous catheter allows for quick access for medications to be administered. The physical exam is done and the blood work is normal and an intravenous catheter is placed, what comes next?
Once the pet is under anesthesia their vitals will be monitored closely to identify any issues. A pulse oximeter is used to monitor the oxygen saturation of the blood. A capnograph is used to measure the CO2 levels to know how well the pet is ventilating. A continuous ECG is used to spot arrhythmias and track heart rate. The pet’s blood pressure will be checked every 3 to 5 minutes to ensure it is not too low which can result in organ damage or too high. The body temperature will be monitored as it is common for pets to become cold while under anesthesia. Active warming with a warm water blanket or heat lamp is commonly used during the procedure to maintain appropriate body temperatures.
Anesthesia requires a variety of medications to be administered, in addition to the inhaled gas. This process is always stressful for the pet owner, but it is also stressful for veterinarians. Our goal is to have the anesthetic procedure be a success and provide the pet with improved quality of life. This is why the above monitoring is so important. If you have a pet that will need have anesthesia, I hope this article gives you a better understanding of what is involved and helps answer any questions you may have. You should always address any concerns or questions with your veterinarian regarding anesthesia prior to the procedure.

With 2018 upon us comes New Year Resolutions. Now would be a great time to include your fur family in these resolutions and start 2018 off right. Below I will discuss some resolutions that you can do with your fur baby.
-
This one is for all pets but especially seniors. Write a bucket list of everything you would like to do with your pet: going to the beach, hiking a particular trail, or passing the canine good citizens test, and make 2018 the year it happens.
-
Update your pet’s identification information. Make sure their tag has a current address, phone number, and microchip number. Also, check the name and address the microchip is registered to and update this information if needed. It’s never too late to be prepared.
-
Start an exercise program. Most New Year Resolutions include improving one’s health in one form or another and this is a great one you can do with your pet. You can start simple, for example, 10 minutes of walking your dog or playing laser tag with your cat a day. Then each week increase this time by 5 minutes or change the activity to keep it exciting. Before you know it you will be exercising with your pet for 45 minutes to an hour a day and loving the extra time together.
-
Along with an exercise program you can improve their health through nutrition. When following the recommended feeding guidelines on various brands of food you are over feeding your pet by 5% to 7%. If your pet is overweight, a good place to start is reducing the amount you currently feed them by 5% to 7%. Also consider what you are feeding them. You should be able to read and understand their food labels the same way you do yours. If there are lots of big, complicated words then stay away from that brand. Our avian friends also benefit from good nutrition. Stay away from all seed diets, these are too fatty and damage the liver. You should feed a good pellet diet with lots of fresh veggies.
-
Start an oral hygiene regime. The best way to slow tartar build up in your pet’s mouth is by brushing their teeth. Ideally, you should brush their teeth daily, but you can start with three times weekly and work towards daily. When brushing their teeth, focus on the lip side of the teeth and use a fluoride free tooth paste.
There are many more resolutions such as providing more mental stimulation with puzzle feeders, make play dates with other pets in your area, beginning a pet savings fund or enroll in a pet insurance plan. Another resolution to celebrate your pet and appreciate the gift they are in your life by taking photos of them or with them. Last, but not least, make a date with the vet if it’s been awhile since your pet’s last exam. Whatever resolution you decide on, start the year on a high note for yourself and your pet!

There are a variety of vaccinations on the market which are all affective but not all equal. Technological advances make some vaccinations safer than others, such as recombinant vaccines that use canary pox virus DNA. There are still vaccinations that use thiomersal (mercury), especially rabies vaccines, as adjuvant (adjuvants are used to inflame the immune system to get a better response). Antibiotics, such as gentamicin, are still used as a preservative in some vaccines.
Pet should be vaccinated based on their risk of exposure versus the risk/benefit of receiving the vaccine. Any pet can have an adverse reaction to any vaccination, these are rare but serious. Reactions can range in severity from mild irritation and swelling at the injection site to anaphylactic shock. The biggest concern regarding vaccinations in cats is Feline Injection-Site Sarcomas, a rare but very aggressive cancer. Feline injection-site sarcomas can occur months to years after vaccination. A recent study suggested that cats with sarcomas in the rear leg were significantly less likely to have received recombinant rabies vaccines than other rabies vaccines.
The American Association of Feline Practitioners Feline Vaccine Advisory Panel makes the following recommendations: The vaccinations that all cats should receive are panleukopenia virus, calicivirus and herpesvirus. Rabies is recommend in areas that is endemic or mandated by law (the state of Arizona does not require you to rabies vaccinate your cat). The feline leukemia vaccination should be considered if your cat ventures outside, although studies have shown that cats greater than one year of age have a 3% chance of contracting feline leukemia if exposed to the virus.
The core vaccinations for dogs are rabies, canine distemper virus, parvovirus, and canine adenovirus. The canine parvovirus and distemper virus mainly affect puppies and younger dogs. These vaccinations save puppies lives each year. After the initial puppies series these vaccinations are recommended every three years. The American Animal Hospital Association Vaccination Guidelines indicate that vaccinations for distemper and parvovirus in healthy canine patients have sustained protective immunity for greater than or equal to five years and greater than seven years for adenovirus. Due to distemper and parvovirus mainly affecting puppies and young dogs, many veterinarians do not recommend continued vaccination for geriatric pets. If you are wondering if your older dog should continue to receive the distemper/parvovirus vaccination speak with your veterinarian.
I encourage you to speak with your veterinarian if you have any questions regarding your pets’ vaccinations.

I am going to broach the difficult topic of end of life decisions. This is a conversion that veterinarians have regularly and I thought that some of you may not be comfortable talking about it. When do you know it is time to say good bye? Does my pet have quality of life? How does the process work? This article will help answer these questions.
Quality of
life comes first. How do you know if
your pet has quality of life? What
defines quality of life is different for each pet. I recommend sitting down and writing the
top 7 to 10 things your pet enjoys doing.
For example; greeting you when you come home, going for walks, laying at
a particular window or spot, and playing
fetch are the items that could define a good quality of life. Then as they begin to not do these things, cross them off the list. Once 70% to 80%
of the items are crossed off, it is a good indication that your pet’s quality of
life is diminishing. Euthanasia should
be considered at this time.
Next, most want to know what to expect during the process. The process is very peaceful. The pet is sedated, placed under anesthesia, prior to the euthanasia. This helps diminish the flight response that some pets will have. This response is a reflex and not painful. After the pet is sedated they will receive an intravenous injection of sodium pentobarbital that will stop the heart. The process only takes seconds to minutes. Their eyes will stay open even after they have passed. During their passing they may urinate or defecate as their body lets go. Once they have passed, you have to consider how you want to handle the remains.
If your pet is euthanized, or if they pass on their own you have a few options. You can have them cremated privately and receive their ashes back, or you can have them cremated with other pets in which the crematorium will handle the ashes. If you chose to bury your pet, you need to know the local laws regarding this, as it is not legal in all areas.
When to euthanize or if euthanasia is the right choice for you is extremely personal. It is normal to feel guilt over making the decision or to feel that the decision isn’t yours to make. I hope this article helps those who aren’t comfortable talking about euthanasia and opens the door for you to be able to discuss this topic further with your veterinarian.
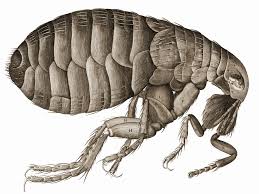
I am sure many of you have seen the reports that the Plague, caused by a bacterium Yersinia pestis , has been found in fleas in Flagstaff. For those of you who have lived in the area for a while you know this is a regular summer occurrence. I’m going to discuss Plague in this month’s article and hopefully put most of you at ease on how best to deal with this.
Yersinia pestis often infects small rodents and is usually transmitted to humans and cats through the bite of an infected flea. Dogs are more resistant to infection and are less likely to show any clinical signs if infected.
There are three times of plague: bubonic, septicemic, and pneumonic. The bubonic form is most common in cats and humans; it also has the lowest mortality rate. The bubonic plague is when the bacteria multiply in the lymph node closest to where it entered the body. The cats this is commonly the lymph nodes under the jaw. The bacteria can then spread to other parts of the body if left untreated with antibiotics. The septicemic plague can form from untreated bubonic plague. Septicemic plague can result from handling an infected animal or being bit by an infected flea. The third form, pneumonic plague, may develop from inhaling infectious droplets or when the bacteria enters the body elsewhere and then spreads to the lungs.
Clinical signs to watch for include: fever, reduced appetite, swelling of the lymph nodes under the jaw or behind the find legs, abscesses, and coughing. If you see these signs and your pet has been outside near rodents then call your veterinarian and have them examined. To help keep your pet safe reduce the rodent habitat around your home. Remove brush, rock piles, junk, and any possible rodent food. Since fleas are the main mode of infection for our pets make sure to use flea control products especially when hiking.
For more information on the Plague visit the CDC website.
Fun fact: to identify doctors treating the plague in the 1300’s, they would wear a hat, mask that was similar to a bird beak, a long gown, and goggles. The beak contained herbs and/or perfumes to help purity the air.

Summer is here, and it is hot! So how do we keep our pets safe during the summer?
Pets can overheat just as easily if not easier than we can. It is very important to have plenty of water available to your pet during the warm months. There are also several products available to help keep your pet cool. They include cooling mats, chilly vests (ice packs can be inserted in the vest to keep your dog cool), popware reusable water bowls and cooling dog boots. Any of these products would be an excellent way to keep your pet cool during outdoor activity.
Signs of heat stroke to watch for:
- Heavy panting
- Dehydration
- Excessive drooling
- Frequent breaks of lying down
- Rapid and irregular heartbeat
- Increased body temperature (above 103 degrees Fahrenheit)
Other signs to watch for: lethargy, diarrhea, vomiting and neurological signs such as stumbling or seizures.
What should you do if your dog is experiencing heat stroke?
- Immediately remove them from the heat
- Offer them cool water
- Cool their body down in cool, but not cold water. Do not submerge their body in water. When using a water hose, reduce the pressure
- Take them to the veterinarian immediately
It is never safe to leave a pet in a car during warmer months. The temperature in a car can rise almost 20 degrees Fahrenheit in just 10 minutes. On a 70-degree day, it can reach 100 degrees in your vehicle. What should you do if you see a dog in a car that is obviously in signs of distress? Gather information about the vehicle (make, model and license plate number), go into nearby businesses and alert their management, if the owner cannot be located call the police or animal control, stay with the dog until help arrives. It is also legal now in the state of Arizona to break the window so that the pet can be safely removed from the hot car.
It is important to keep pets safe in the summer. As long as you are aware of the signs of heat stress in pets and are prepared in case of an emergency, the summer will be a breeze. Get out the kiddie pools and frosty paws and let the summer fun begin.
Nutrition is one of the most important preventative measures we have to help our pets stay healthy. There are many diseases that we can treat with proper nutrition. With this month’s article I’d like to discuss feline nutrition in particular.
Cats are obligate carnivores. This means the physiology and anatomy of the cat are suited to eating a high protein, meat diet. Dry food is too high in carbohydrates and too low in protein for cats. Many pet parents feed a dry food believing that it is better for their feline’s teeth. This is simply not true. Dry food is not abrasive enough to clean or reduce the dental calculus from building up on the teeth.
Kidney disease, diabetes, and hyperthyroidism are diseases veterinarians see on a daily bases. They can also all be managed with proper nutrition. The progression of kidney disease is significantly slowed with a low phosphorus diet. Cats with kidney disease need protein to help maintain muscle mass, and protein restriction is generally not recommended depending on the affected feline. Nutrition is one of the most important factors when treating a cat with compromised kidneys.
The majority of diabetic cats can be weaned off insulin with appropriate diet changes. A high protein, low-carbohydrate diet has been associated with remission of diabetes in cats. This is achieved through a variety of canned foods or you can cook a at home diet as well. You can also cook for a cat with hyperthyroidism to help control the thyroid.
Cats with hyperthyroidism are in a elevated metabolic state. They need higher protein, higher fat, and a lower carbohydrate content than cats without hyperthyroidism. In addition to increasing the protein and fat, the iodine can be significantly reduced. With reduced iodine, the thyroid gland doesn’t have what it needs to make the thyroid hormones which create the elevated metabolic state. To achieve the low iodine diet, you can do a at home cooked diet or there is a prescription diet available. Most over the counter diets available are too high in iodine.
For all ailments there are medical therapies to improve your cat's quality of life and slow the disease progression. But without nutrition, the medical therapies are incomplete.
If you are interested in learning more about how nutrition can help your pet talk with your veterinarian.